The Michigan maternal mortality rate was 16.4 per 100,000 live births in 2018, according to the National Center for Health Statistics. At the national level in 2017 the maternal mortality rate was 17.4 per 100,000 live births. While Michigan’s numbers were slightly less than the national average, they are still concerning, especially considering the United States has among the highest maternal mortality rates across amongst other nations.
Maternal deaths include deaths of women while pregnant or within 42 days of termination of pregnancy irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.
Understanding, and improving, maternal mortality is important because it helps highlight the effectiveness of the country’s health care system as it relates to general, obstetric and infant care, and is also a human rights issue, as everyone deserves quality and equal care.
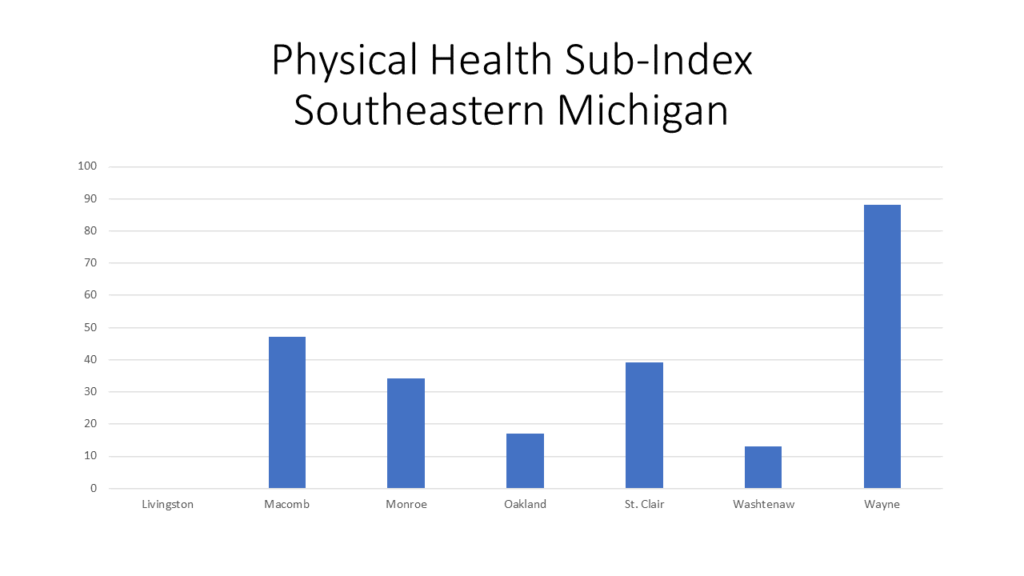
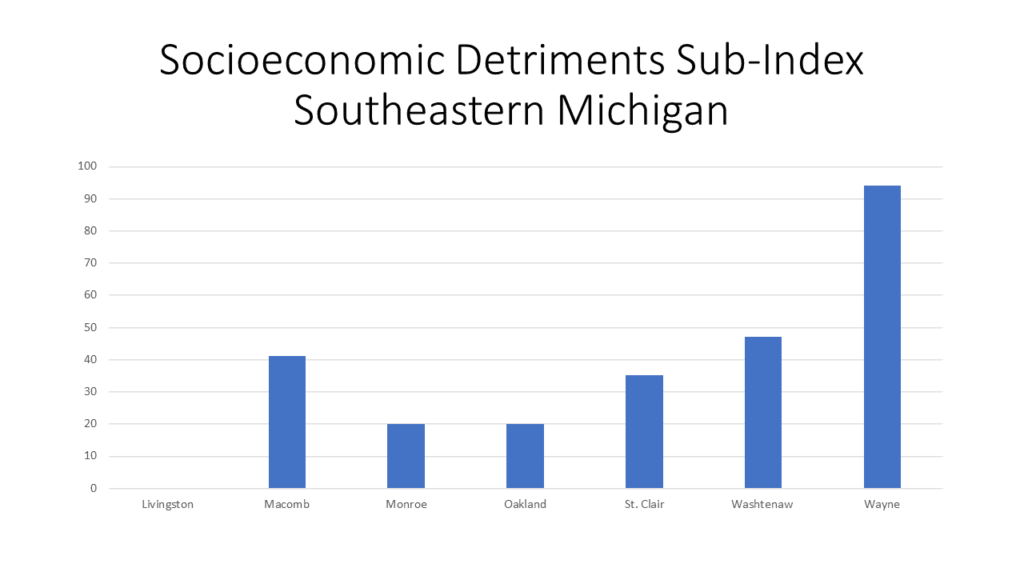
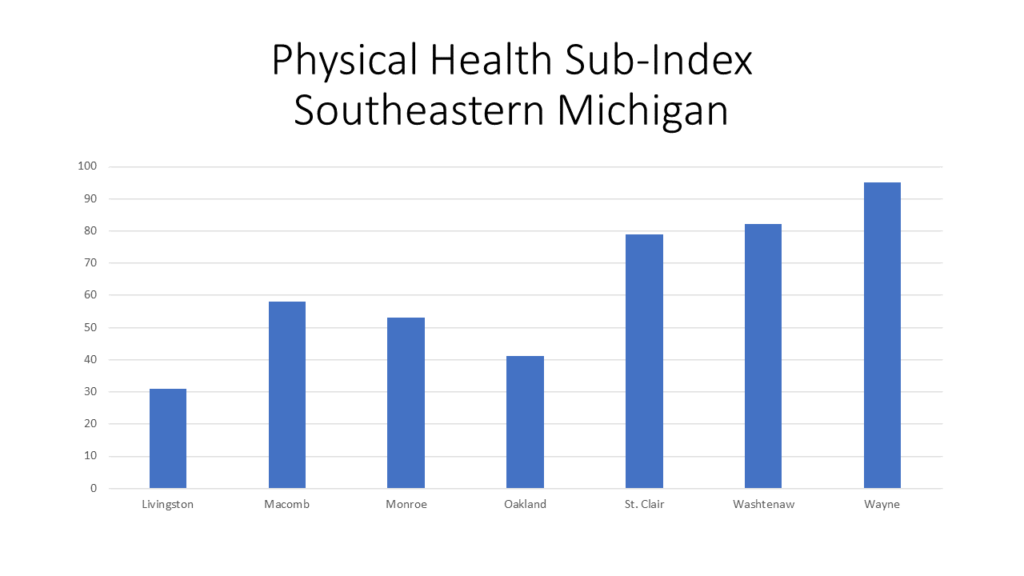
In the graphs below we show what factors impact maternal mortality rates and maternal health in general. Several factors, based off maternal health and community data, were combined by Surgo Ventures, a privately funded action tank, to create the Maternal Vulnerability Index (MVI). This index represents six categories, or sub-indexes, in total: Reproductive Healthcare, Physical Health, Mental Health and Substance Abuse, General Healthcare, Socioeconomic Detriments and Physical Environment. In Southeastern Michigan, and throughout the country, each county and states ranks differently in each category, with the higher number meaning there is an increased vulnerability. This report does not have a national index for the sub-indexes or the MVI as a whole for comparison. The highest level for comparison is at the state level.
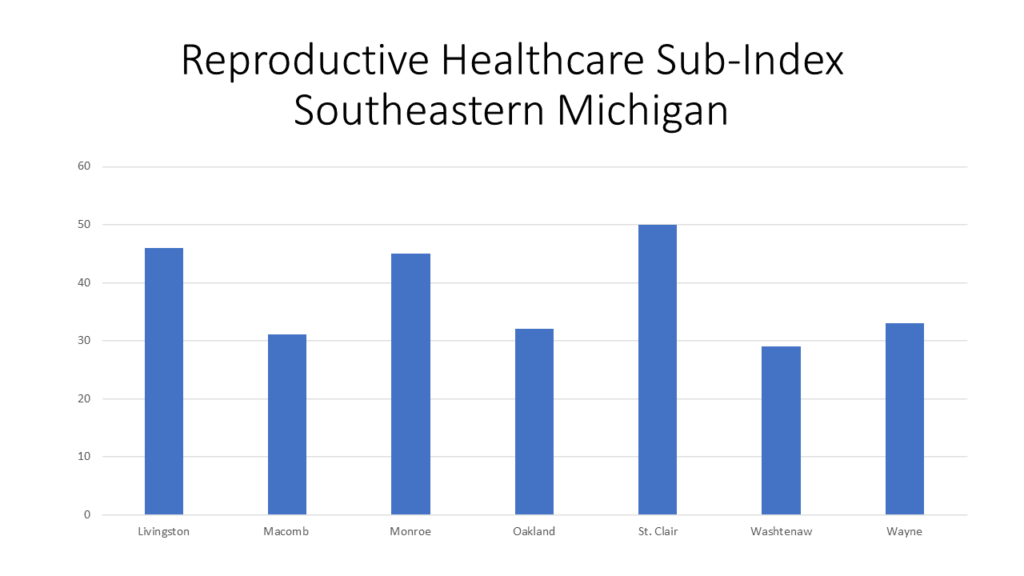
The Reproductive Healthcare factor in the MVI is based off a woman’s access to family planning and reproductive services, as well as availability of skilled attendants. As with all the data discussed in this post, the vulnerability level varies greatly by location (again, higher numbers refer to higher vulnerability). In Southeastern Michigan, St. Clair County has the highest Reproductive Healthcare MVI Sub-Index at 50, while nationally there are counties in the Dakotas, Texas, Arkansas, Missouri, Nebraska and several other states where the Reproductive Healthcare Sub-Index is above 85. The State of Michigan has a Reproductive Healthcare Sub-Index factor of 68. Texas has the highest Reproductive Healthcare Sub-Index of 100 of all 50 states.
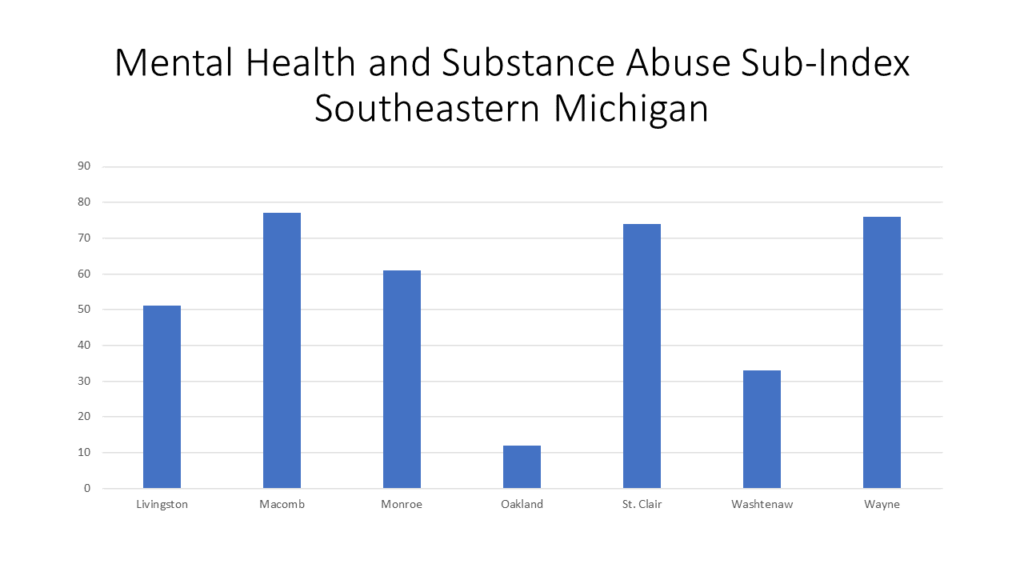
The Mental Health and Substance Abuse Sub-Index is among one of the higher ones for counties in Michigan, with five of the seven in Southeastern Michigan having a vulnerability index above 50. Macomb County has the highest vulnerability index in the region at 77, followed by Wayne County with an index of 76 and St. Clair County with an index of 74. Michigan has a Mental Health and Substance Abuse Sub-Index of 62 and the State with the highest sub-index is West Virginia at 100. The indicators that play into this index include stress, access to mental health and substance abuse institutions and the overall mental health of mothers in the area.
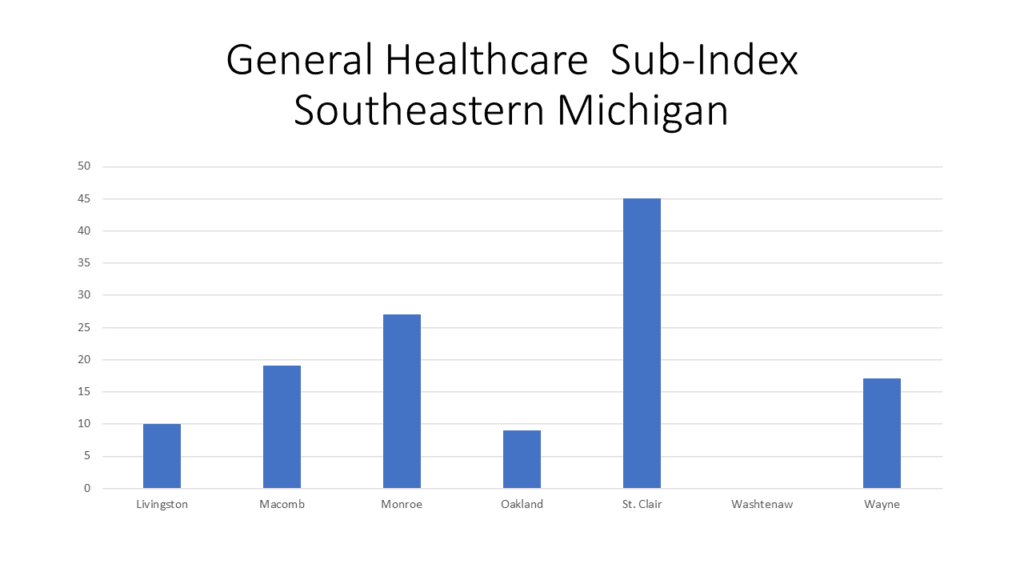
St. Clair County has the highest vulnerability index at 45 while Washtenaw County has an index of 0, meaning there is ease in access to and affordability of healthcare for reproductive age women. Michigan has a General Healthcare Sub-Index of 29, and comparatively, the two states with the highest sub-index are Mississippi and Alabama at 100.
St. Clair County has the highest vulnerability index at 45 while Washtenaw County has an index of 0, meaning there is ease in access to and affordability of healthcare for reproductive age women. Michigan has a General Healthcare Sub-Index of 29, and comparatively, the two states with the highest sub-index are Mississippi and Alabama at 100.
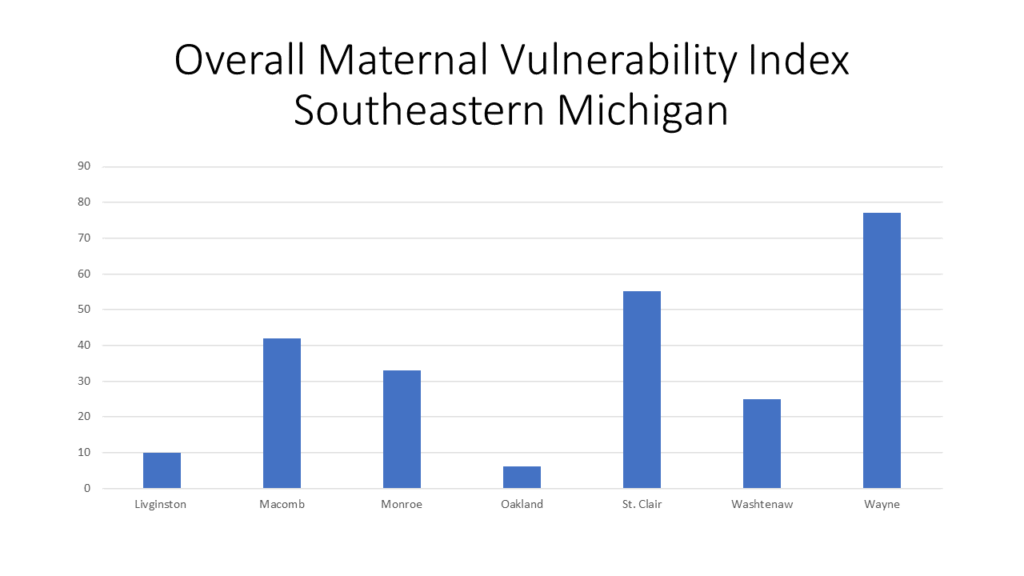
In examining the factors above, it should go without saying that race, socioeconomic status and location are all overarching factors into the MVI. This is examined on a deeper level through the index though and will be further discussed in an upcoming post.